
Insulin resistance: why fasting insulin is the best early test
August 5, 2025
Millions of people unknowingly live with insulin resistance, a silent precursor to type 2 diabetes that can develop years before high blood sugar is detected. Traditional tests like fasting glucose and HbA1c often miss early warning signs, but fasting insulin tests can reveal metabolic issues much sooner.
Key takeaways:
- Insulin resistance affects around 35% of Australian adults and an estimated 26% of adults worldwide, with U.S. data showing 40% of adults aged 18–44 impacted.
- Fasting insulin levels above 10–15 mIU/L may signal early metabolic dysfunction, even when glucose and HbA1c levels appear normal.
- Lifestyle changes, including diet, exercise, and sleep, can improve insulin sensitivity, especially when guided by tools like fasting insulin tests and continuous glucose monitoring (CGM).
Fasting insulin testing offers a critical advantage: it identifies early risks, enabling interventions before long-term damage occurs. Pairing it with CGM provides real-time insights into how daily habits impact your glucose levels, empowering you to take control of your metabolic health.
If you're wondering what causes insulin resistance and how it develops, for more info check out insulin resistance and its causes to learn about key risk factors and ways to support better metabolic health.
What is insulin resistance, and why should you care?
Insulin resistance impacts an estimated 70–80 million people in the United States. Alarmingly, studies show that 40% of adults aged 18–44 are affected by this condition. Despite being so common, it remains one of the most underdiagnosed health issues, leaving many unaware of its long-term consequences.
At its core, insulin resistance occurs when your muscle, fat, and liver cells stop responding properly to insulin. This sets off a chain reaction of metabolic issues that can quietly harm your health over time.
How insulin resistance works
Insulin, produced by the pancreas, plays a critical role in managing blood sugar levels. It helps move sugar from your bloodstream into your cells, where it’s used for energy. But when your cells become resistant to insulin, the pancreas compensates by producing more of it. Despite this, sugar continues to build up in your blood.
This creates a cycle of elevated blood sugar (hyperglycemia) and excess insulin production, which can lead to long-term health problems.
Excess sugar in the blood is stored in the liver and muscles. Once these storage areas are full, the body converts the remaining sugar into fat, which can contribute to weight gain. The main areas affected by insulin resistance are skeletal muscle, the liver, and fat tissue.
When these systems fail to work together, your body’s ability to regulate blood sugar starts to break down. This breakdown not only raises blood sugar levels but also increases the risk of diabetes and heart disease.
Link to type 2 diabetes and metabolic syndrome
Insulin resistance is a key factor in the development of type 2 diabetes, often appearing 10 to 15 years before diabetes is officially diagnosed. During this time, the body struggles to manage blood sugar, leading to excess insulin production (hyperinsulinemia). Eventually, the pancreas can no longer keep up, resulting in persistent high blood sugar and, ultimately, type 2 diabetes.
But the risks don’t stop there. Insulin resistance is also closely tied to metabolic syndrome, a condition that affects about 1 in 3 adults in the United States. Metabolic syndrome increases the likelihood of heart disease and other serious health concerns. It’s diagnosed when a person has at least three of the following: abdominal obesity, high blood pressure, high triglycerides, low HDL cholesterol, or impaired fasting glucose.
Insulin resistance is often at the center of these issues, contributing to complications like high blood sugar, high blood pressure, abnormal cholesterol levels, and inflammation.
Certain groups face even higher risks. For example, Hispanic individuals in the United States are particularly vulnerable to developing metabolic syndrome.
The good news? Insulin resistance can be addressed. There are ways to make your cells more responsive to insulin. Regular physical activity, losing weight (if needed), and eating a balanced diet can all improve insulin sensitivity. Even modest weight loss can make a difference, helping to lower blood pressure and enhance how your body uses insulin.
Diabetes tests compared: what works best
Early detection plays a key role in preventing irreversible metabolic damage, yet not all tests are equally effective at identifying early signs of trouble. Many healthcare providers rely on traditional markers like fasting glucose and HbA1c, but these often fail to catch the earliest signs of metabolic dysfunction.
Understanding how these tests work and their limitations can help you make smarter choices when it comes to health screenings. Let’s break down how these tests compare and why their differences matter.
Fasting glucose and HbA1c: how they work
Fasting blood glucose (FBS) measures your blood sugar levels after an eight-hour fast. It’s one of the most commonly used tests for diagnosing diabetes. A result of 126 mg/dL or higher typically indicates diabetes, while levels between 100 and 125 mg/dL suggest prediabetes. Anything below 100 mg/dL is considered normal.
HbA1c, on the other hand, measures your average blood sugar levels over the past two to three months. A reading of 6.5% or higher signals diabetes, while levels between 5.7% and 6.4% point to prediabetes. Normal levels fall below 5.7%. The advantage of HbA1c? It doesn’t require fasting and gives a broader view of your blood sugar trends over time.
However, both fasting glucose and HbA1c have a major drawback: they usually detect issues only after significant metabolic damage has already occurred. Research shows that elevated insulin levels can precede high glucose levels by as much as 13 years, and hyperinsulinemia can signal glycemic dysfunction up to 24 years in advance.
Fasting insulin: a better tool for early detection
Fasting insulin measures the amount of insulin in your blood after an overnight fast, typically reported in microunits per milliliter (mIU/L). While there’s no universal agreement on what’s optimal, most labs consider 2–20 mIU/L to be the normal range. Many experts argue that levels above 10–15 mIU/L may indicate early insulin resistance.
This test stands out because it can detect metabolic issues well before fasting glucose or HbA1c levels show abnormalities. Studies have revealed that fasting insulin testing uncovers early signs of insulin resistance, offering a critical opportunity for intervention.
For instance, one study found that 30.5% of young adults had hyperinsulinemia despite normal glucose and HbA1c levels. Even among those with HbA1c below 5.7%, 10.5% had fasting insulin levels exceeding 15 mIU/L.
Insulin resistance forces the pancreas to work harder, producing more insulin to keep blood sugar levels stable. This elevated insulin becomes detectable long before blood sugar rises, making fasting insulin a strong predictor of future diabetes.
Test comparison: fasting glucose vs. HbA1c vs. fasting insulin
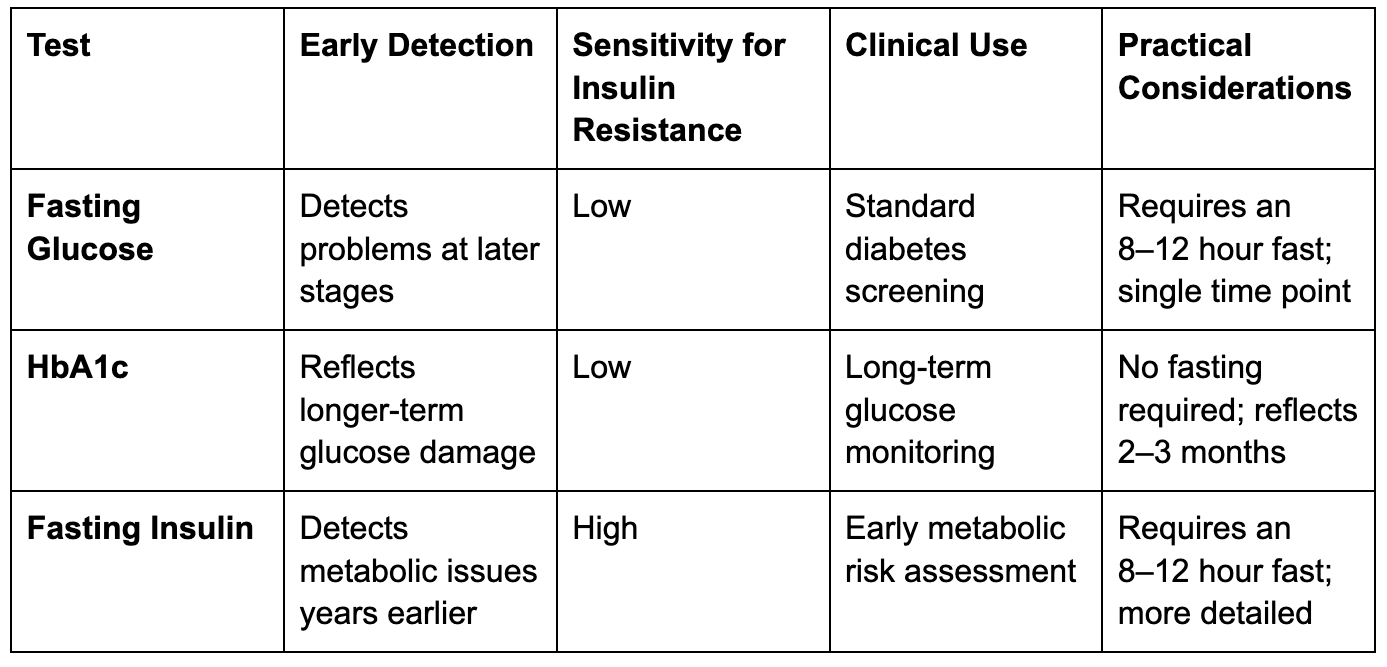
The table above emphasises fasting insulin’s ability to reveal early metabolic changes. Research indicates that insulin levels are more closely tied to metabolic syndrome traits than HbA1c, except when it comes to hyperglycaemia.
One large study found that 40% of participants showed signs of insulin resistance and pancreatic strain even though they didn’t meet the standard criteria for prediabetes. This means many people with normal glucose and HbA1c levels may already have significant metabolic dysfunction—something fasting insulin can identify more reliably.
A large number of Americans remain undiagnosed with insulin resistance because traditional glucose-based tests often miss the mark. While each test has its role, fasting insulin provides the earliest glimpse into metabolic health issues. Catching insulin resistance early allows for timely lifestyle changes and ongoing monitoring, which can help prevent the progression to diabetes.
Ever wondered what early signs your metabolic health might be sending you? Discover five red flags to watch for and what you can do about them in 5 signs your metabolic health needs attention and how to fix it.
How Continuous Glucose Monitoring helps
Fasting insulin tests provide a quick snapshot of your health, but continuous glucose monitoring (CGM) takes things further by offering a real-time view of your glucose levels. Together, these tools can help detect and address insulin sensitivity issues early, before they escalate into more serious problems.
Now, let’s dive into how CGM works and why it’s so beneficial.
CGM basics and benefits
Continuous glucose monitoring is a wearable device that tracks glucose levels throughout the day and night. Unlike traditional finger-prick tests, which provide single data points, CGM gives a continuous stream of information, revealing patterns and trends. The device measures glucose in the interstitial fluid, which typically lags about 15 minutes behind blood glucose levels.
This constant tracking offers several advantages. It minimises the need for frequent finger sticks, helps you spot trends like post-meal spikes, and allows for timely adjustments to manage your levels more effectively.
For example, you might notice that your usual breakfast leads to a glucose spike or that a quick walk after lunch helps stabilise your levels. Plus, the data can be downloaded and shared with your healthcare provider, paving the way for tailored advice and better care.
Lifestyle changes to improve insulin sensitivity
Making lifestyle adjustments can help reverse insulin resistance, especially when combined with tools like fasting insulin tests and continuous glucose monitoring (CGM). These changes create a tailored approach to improving metabolic health.
Diet changes for better insulin function
Your diet plays a major role in managing insulin sensitivity. The goal is to make thoughtful swaps that help regulate blood sugar levels while reducing stress on your insulin-producing cells.
Start by cutting out refined carbohydrates like white bread, sugary drinks, and processed snacks that cause blood sugar spikes. Instead, choose low-glycaemic-index foods such as whole grains, legumes, and non-starchy vegetables.
Increasing your fibre intake is another effective strategy. Foods like oats, barley, fibrous vegetables, and fruits slow glucose absorption and support overall metabolic health. Additionally, replace saturated fats with healthier unsaturated fats found in olive oil, avocados, nuts, seeds, and fatty fish.
Meal composition matters. Pairing carbohydrates with protein or healthy fats can prevent sharp blood sugar spikes. For example, enjoy an apple with almond butter or mix lean protein and vegetables into your pasta dish for a balanced meal.
Interestingly, even artificial sweeteners can affect insulin sensitivity. A 2020 study in Cell Metabolism found that consuming sucralose with carbohydrates reduced insulin sensitivity in healthy participants. This underscores the importance of prioritising whole, minimally processed foods.
Monitor your progress. Regular fasting insulin tests can track how your body responds to dietary changes. For instance, reducing refined carbs may lead to noticeable improvements in just a few weeks.
While diet is essential, other lifestyle factors like exercise, sleep, and stress management are equally important for improving insulin sensitivity.
Exercise, sleep, and stress management
Diet often takes centre stage, but exercise, quality sleep, and stress management are just as critical for maintaining insulin sensitivity. These elements work together to support or hinder your metabolic health.
Exercise is a powerful tool for improving insulin function. Studies show that increasing weekly physical activity by just 500 calories reduces the risk of type 2 diabetes by about 9%. High-intensity interval training (HIIT) is particularly effective, especially for those dealing with poor sleep.
But you don’t need to go all out – simple habits like walking more, taking the stairs, or standing periodically throughout the day can make a real difference.
Stress is another factor to watch. Chronic stress raises cortisol levels, which interferes with insulin function and often leads to poor sleep. This creates a cycle where stress and poor sleep feed into each other, worsening insulin sensitivity.
Start small. Commit to a 20-minute walk after dinner, set a consistent bedtime, or practise 10 minutes of deep breathing daily. These small steps often build on each other, creating a positive cycle of improved habits.
Combining fasting insulin tests with CGM data
Pairing lifestyle changes with precise monitoring tools like fasting insulin tests and CGM provides a clearer picture of your metabolic health. Together, they offer insights that help fine-tune your approach.
Fasting insulin tests establish a baseline. When fasting plasma glucose levels exceed 4.9 mmol/L (about 88 mg/dL), the risk of insulin resistance and, consequently, diabetes doubles. This test gives you a concrete target to work toward with your lifestyle changes.
CGM fills in the gaps. While fasting tests provide a snapshot, CGM tracks glucose levels throughout the day. For example, you might learn that certain meals cause prolonged glucose spikes or that stress at work consistently raises your blood sugar in the afternoon. This real-time data helps you identify which interventions work best for your body.
Tailored diets based on post-meal glucose responses are more effective than generic plans. CGM data allows you to see exactly which foods and combinations stabilise your glucose levels.
AI technology takes this a step further. Modern CGM systems can use AI to analyse patterns and predict glucose levels. A pilot study in rural India showed that AI-driven interventions improved glycaemic control in prediabetic individuals by 18%. While this technology is still advancing, it highlights how data-driven insights can lead to more personalised strategies.
If you're wondering how to reverse insulin resistance and boost sensitivity, check out how to reverse insulin resistance insulin sensitivity for practical steps.
How Vively can help you spot and manage insulin resistance
Understanding insulin resistance early is key, and pairing fasting insulin tests with continuous monitoring gives you a clearer picture of your metabolic health. Vively provides real-time insights with continuous glucose monitoring (CGM), helping you see how your meals, movement, sleep, and stress impact your glucose levels throughout the day.
With Vively, you can:
- Track your daily glucose patterns to identify spikes and trends linked to insulin resistance.
- Get personalised guidance from an accredited dietitian to improve insulin sensitivity through diet and lifestyle changes.
- Monitor your progress over time, so you can take action before blood sugar or HbA1c levels rise.
By combining early testing with Vively’s CGM insights and expert support, you gain the tools to prevent long-term complications and take control of your metabolic health.
Take control of your metabolic health
Fasting insulin testing can reveal metabolic issues long before traditional markers like blood glucose and HbA1c show any signs. The numbers don't lie: in a study of 1,313 young adults, 30.5% had elevated insulin levels despite having normal blood glucose and HbA1c readings.
Even more surprising, among those with HbA1c under 5.7%, a range typically considered healthy, 10.5% still had fasting insulin levels above 15 mIU/L. This means that nearly 1 in 10 people labelled as "healthy" by standard tests were already showing early signs of insulin resistance.
Fasting insulin testing is far more sensitive than HbA1c or fasting glucose at detecting early resistance. HbA1c has a sensitivity of just 49%, while fasting glucose is even lower at 25%. These statistics highlight the value of integrating fasting insulin testing and continuous monitoring into your health routine.
When combined with continuous glucose monitoring (CGM), fasting insulin results can guide meaningful lifestyle changes. For example, a study of 2,217 participants using remote CGM saw improvements in hyperglycaemia, glucose variability, and even weight management.
Programs like Vively's CGM system make this process even more effective. By pairing real-time glucose tracking with personalised nutrition coaching, you can see exactly how your diet, exercise, and sleep habits impact your glucose levels. The coaching helps translate this data into practical, sustainable changes tailored to your body's unique needs.
It's also worth noting that a fasting plasma glucose level above 88 mg/dL (4.9 mmol/L) doubles your risk of insulin resistance. But you don’t need to wait for your levels to reach that point. Early lifestyle changes like the diet tweaks, exercise plans, and sleep strategies mentioned earlier – can significantly lower your risk of progressing to type 2 diabetes.
With clear early warning signs and actionable data, you have the tools to take charge of your metabolic health. A fasting insulin test, paired with CGM insights, can help you fine-tune your habits before lasting damage occurs. This proactive approach works seamlessly with lifestyle adjustments to reverse insulin resistance and keep type 2 diabetes at bay.
Your metabolic health is largely in your hands. The key is having the right information at the right time. Fasting insulin testing gives you that critical early insight, empowering you to act when it matters most.
FAQs
Why is fasting insulin a better early indicator of insulin resistance than fasting glucose or HbA1c?
Fasting insulin serves as a stronger early indicator of insulin resistance because it can reveal problems long before blood sugar levels or HbA1c begin to climb. Insulin resistance tends to develop slowly, and fasting insulin is often one of the first markers to signal that something is off.
Catching insulin resistance early allows for timely action to improve metabolic health and lower the chances of progressing to diabetes. On the other hand, fasting glucose and HbA1c usually only flag issues after blood sugar control has already been significantly disrupted.
How can changes to your diet and exercise routine improve insulin sensitivity and help manage or reverse insulin resistance?
Improving how your body responds to insulin often begins with small, manageable lifestyle changes. Regular exercise, whether it's walking, swimming, strength training, or yoga can make a big difference in how efficiently your body uses insulin. Try to aim for at least 150 minutes of moderate activity each week to see positive effects.
Your diet plays a key role too. Prioritise whole, nutrient-packed foods like vegetables, fruits, lean proteins, healthy fats, and fibre-rich options such as whole grains and legumes. Cutting back on added sugars and processed foods can also help keep your blood sugar steady and support better overall metabolic health.
By weaving these habits into your daily life, you can take meaningful steps toward managing blood sugar and reducing the risk of diabetes in the long run.
How does continuous glucose monitoring (CGM) help with understanding and managing insulin resistance?
Continuous glucose monitoring (CGM) offers real-time updates on how your blood sugar levels change during the day. By observing these trends, CGMs can reveal early indicators of insulin resistance, often before it becomes apparent through standard tests like fasting glucose or HbA1c.
With this information, you can tailor your diet, exercise routine, and daily habits to improve blood sugar control and lower the chances of developing diabetes. CGMs serve as a powerful resource for spotting issues early and taking charge of your metabolic health.
Why is fasting insulin a better early indicator of insulin resistance than fasting glucose or HbA1c?
Fasting insulin serves as a stronger early indicator of insulin resistance because it can reveal problems long before blood sugar levels or HbA1c begin to climb. Insulin resistance tends to develop slowly, and fasting insulin is often one of the first markers to signal that something is off.
Catching insulin resistance early allows for timely action to improve metabolic health and lower the chances of progressing to diabetes. On the other hand, fasting glucose and HbA1c usually only flag issues after blood sugar control has already been significantly disrupted.
How can changes to your diet and exercise routine improve insulin sensitivity and help manage or reverse insulin resistance?
Improving how your body responds to insulin often begins with small, manageable lifestyle changes. Regular exercise, whether it's walking, swimming, strength training, or yoga, can make a big difference in how efficiently your body uses insulin. Try to aim for at least 150 minutes of moderate activity each week to see positive effects.
Your diet plays a key role too. Prioritise whole, nutrient-packed foods like vegetables, fruits, lean proteins, healthy fats, and fibre-rich options such as whole grains and legumes. Cutting back on added sugars and processed foods can also help keep your blood sugar steady and support better overall metabolic health.
By weaving these habits into your daily life, you can take meaningful steps toward managing blood sugar and reducing the risk of diabetes in the long run.
How does continuous glucose monitoring (CGM) help with understanding and managing insulin resistance?
Continuous glucose monitoring (CGM) offers real-time updates on how your blood sugar levels change during the day. By observing these trends, CGMs can reveal early indicators of insulin resistance, often before it becomes apparent through standard tests like fasting glucose or HbA1c.
With this information, you can tailor your diet, exercise routine, and daily habits to improve blood sugar control and lower the chances of developing diabetes. CGMs serve as a powerful resource for spotting issues early and taking charge of your metabolic health.
Meet our team.
Subscribe to our newsletter & join a community of 20,000+ Aussies
Get access to limited content drops, free invites to expert fireside chats, and exclusive offers.

Insulin resistance: why fasting insulin is the best early test
Millions of people unknowingly live with insulin resistance, a silent precursor to type 2 diabetes that can develop years before high blood sugar is detected. Traditional tests like fasting glucose and HbA1c often miss early warning signs, but fasting insulin tests can reveal metabolic issues much sooner.
Key takeaways:
- Insulin resistance affects around 35% of Australian adults and an estimated 26% of adults worldwide, with U.S. data showing 40% of adults aged 18–44 impacted.
- Fasting insulin levels above 10–15 mIU/L may signal early metabolic dysfunction, even when glucose and HbA1c levels appear normal.
- Lifestyle changes, including diet, exercise, and sleep, can improve insulin sensitivity, especially when guided by tools like fasting insulin tests and continuous glucose monitoring (CGM).
Fasting insulin testing offers a critical advantage: it identifies early risks, enabling interventions before long-term damage occurs. Pairing it with CGM provides real-time insights into how daily habits impact your glucose levels, empowering you to take control of your metabolic health.
If you're wondering what causes insulin resistance and how it develops, for more info check out insulin resistance and its causes to learn about key risk factors and ways to support better metabolic health.
What is insulin resistance, and why should you care?
Insulin resistance impacts an estimated 70–80 million people in the United States. Alarmingly, studies show that 40% of adults aged 18–44 are affected by this condition. Despite being so common, it remains one of the most underdiagnosed health issues, leaving many unaware of its long-term consequences.
At its core, insulin resistance occurs when your muscle, fat, and liver cells stop responding properly to insulin. This sets off a chain reaction of metabolic issues that can quietly harm your health over time.
How insulin resistance works
Insulin, produced by the pancreas, plays a critical role in managing blood sugar levels. It helps move sugar from your bloodstream into your cells, where it’s used for energy. But when your cells become resistant to insulin, the pancreas compensates by producing more of it. Despite this, sugar continues to build up in your blood.
This creates a cycle of elevated blood sugar (hyperglycemia) and excess insulin production, which can lead to long-term health problems.
Excess sugar in the blood is stored in the liver and muscles. Once these storage areas are full, the body converts the remaining sugar into fat, which can contribute to weight gain. The main areas affected by insulin resistance are skeletal muscle, the liver, and fat tissue.
When these systems fail to work together, your body’s ability to regulate blood sugar starts to break down. This breakdown not only raises blood sugar levels but also increases the risk of diabetes and heart disease.
Link to type 2 diabetes and metabolic syndrome
Insulin resistance is a key factor in the development of type 2 diabetes, often appearing 10 to 15 years before diabetes is officially diagnosed. During this time, the body struggles to manage blood sugar, leading to excess insulin production (hyperinsulinemia). Eventually, the pancreas can no longer keep up, resulting in persistent high blood sugar and, ultimately, type 2 diabetes.
But the risks don’t stop there. Insulin resistance is also closely tied to metabolic syndrome, a condition that affects about 1 in 3 adults in the United States. Metabolic syndrome increases the likelihood of heart disease and other serious health concerns. It’s diagnosed when a person has at least three of the following: abdominal obesity, high blood pressure, high triglycerides, low HDL cholesterol, or impaired fasting glucose.
Insulin resistance is often at the center of these issues, contributing to complications like high blood sugar, high blood pressure, abnormal cholesterol levels, and inflammation.
Certain groups face even higher risks. For example, Hispanic individuals in the United States are particularly vulnerable to developing metabolic syndrome.
The good news? Insulin resistance can be addressed. There are ways to make your cells more responsive to insulin. Regular physical activity, losing weight (if needed), and eating a balanced diet can all improve insulin sensitivity. Even modest weight loss can make a difference, helping to lower blood pressure and enhance how your body uses insulin.
Diabetes tests compared: what works best
Early detection plays a key role in preventing irreversible metabolic damage, yet not all tests are equally effective at identifying early signs of trouble. Many healthcare providers rely on traditional markers like fasting glucose and HbA1c, but these often fail to catch the earliest signs of metabolic dysfunction.
Understanding how these tests work and their limitations can help you make smarter choices when it comes to health screenings. Let’s break down how these tests compare and why their differences matter.
Fasting glucose and HbA1c: how they work
Fasting blood glucose (FBS) measures your blood sugar levels after an eight-hour fast. It’s one of the most commonly used tests for diagnosing diabetes. A result of 126 mg/dL or higher typically indicates diabetes, while levels between 100 and 125 mg/dL suggest prediabetes. Anything below 100 mg/dL is considered normal.
HbA1c, on the other hand, measures your average blood sugar levels over the past two to three months. A reading of 6.5% or higher signals diabetes, while levels between 5.7% and 6.4% point to prediabetes. Normal levels fall below 5.7%. The advantage of HbA1c? It doesn’t require fasting and gives a broader view of your blood sugar trends over time.
However, both fasting glucose and HbA1c have a major drawback: they usually detect issues only after significant metabolic damage has already occurred. Research shows that elevated insulin levels can precede high glucose levels by as much as 13 years, and hyperinsulinemia can signal glycemic dysfunction up to 24 years in advance.
Fasting insulin: a better tool for early detection
Fasting insulin measures the amount of insulin in your blood after an overnight fast, typically reported in microunits per milliliter (mIU/L). While there’s no universal agreement on what’s optimal, most labs consider 2–20 mIU/L to be the normal range. Many experts argue that levels above 10–15 mIU/L may indicate early insulin resistance.
This test stands out because it can detect metabolic issues well before fasting glucose or HbA1c levels show abnormalities. Studies have revealed that fasting insulin testing uncovers early signs of insulin resistance, offering a critical opportunity for intervention.
For instance, one study found that 30.5% of young adults had hyperinsulinemia despite normal glucose and HbA1c levels. Even among those with HbA1c below 5.7%, 10.5% had fasting insulin levels exceeding 15 mIU/L.
Insulin resistance forces the pancreas to work harder, producing more insulin to keep blood sugar levels stable. This elevated insulin becomes detectable long before blood sugar rises, making fasting insulin a strong predictor of future diabetes.
Test comparison: fasting glucose vs. HbA1c vs. fasting insulin
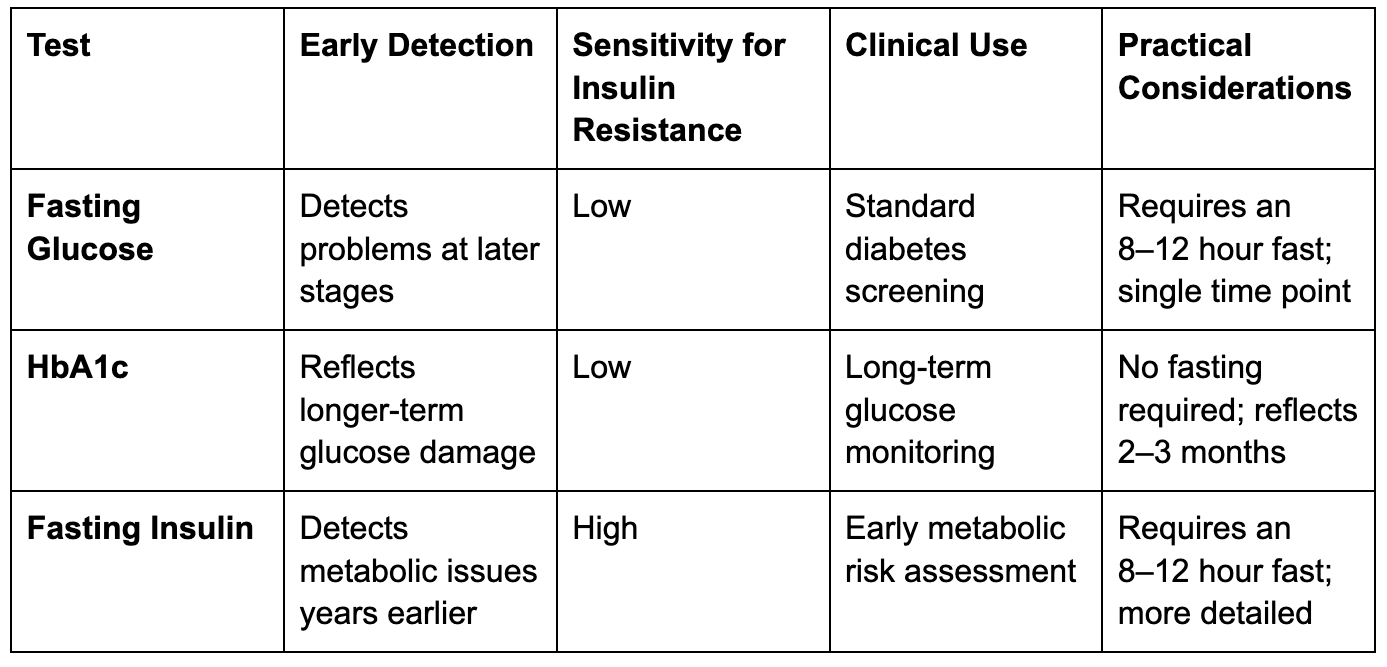
The table above emphasises fasting insulin’s ability to reveal early metabolic changes. Research indicates that insulin levels are more closely tied to metabolic syndrome traits than HbA1c, except when it comes to hyperglycaemia.
One large study found that 40% of participants showed signs of insulin resistance and pancreatic strain even though they didn’t meet the standard criteria for prediabetes. This means many people with normal glucose and HbA1c levels may already have significant metabolic dysfunction—something fasting insulin can identify more reliably.
A large number of Americans remain undiagnosed with insulin resistance because traditional glucose-based tests often miss the mark. While each test has its role, fasting insulin provides the earliest glimpse into metabolic health issues. Catching insulin resistance early allows for timely lifestyle changes and ongoing monitoring, which can help prevent the progression to diabetes.
Ever wondered what early signs your metabolic health might be sending you? Discover five red flags to watch for and what you can do about them in 5 signs your metabolic health needs attention and how to fix it.
How Continuous Glucose Monitoring helps
Fasting insulin tests provide a quick snapshot of your health, but continuous glucose monitoring (CGM) takes things further by offering a real-time view of your glucose levels. Together, these tools can help detect and address insulin sensitivity issues early, before they escalate into more serious problems.
Now, let’s dive into how CGM works and why it’s so beneficial.
CGM basics and benefits
Continuous glucose monitoring is a wearable device that tracks glucose levels throughout the day and night. Unlike traditional finger-prick tests, which provide single data points, CGM gives a continuous stream of information, revealing patterns and trends. The device measures glucose in the interstitial fluid, which typically lags about 15 minutes behind blood glucose levels.
This constant tracking offers several advantages. It minimises the need for frequent finger sticks, helps you spot trends like post-meal spikes, and allows for timely adjustments to manage your levels more effectively.
For example, you might notice that your usual breakfast leads to a glucose spike or that a quick walk after lunch helps stabilise your levels. Plus, the data can be downloaded and shared with your healthcare provider, paving the way for tailored advice and better care.
Lifestyle changes to improve insulin sensitivity
Making lifestyle adjustments can help reverse insulin resistance, especially when combined with tools like fasting insulin tests and continuous glucose monitoring (CGM). These changes create a tailored approach to improving metabolic health.
Diet changes for better insulin function
Your diet plays a major role in managing insulin sensitivity. The goal is to make thoughtful swaps that help regulate blood sugar levels while reducing stress on your insulin-producing cells.
Start by cutting out refined carbohydrates like white bread, sugary drinks, and processed snacks that cause blood sugar spikes. Instead, choose low-glycaemic-index foods such as whole grains, legumes, and non-starchy vegetables.
Increasing your fibre intake is another effective strategy. Foods like oats, barley, fibrous vegetables, and fruits slow glucose absorption and support overall metabolic health. Additionally, replace saturated fats with healthier unsaturated fats found in olive oil, avocados, nuts, seeds, and fatty fish.
Meal composition matters. Pairing carbohydrates with protein or healthy fats can prevent sharp blood sugar spikes. For example, enjoy an apple with almond butter or mix lean protein and vegetables into your pasta dish for a balanced meal.
Interestingly, even artificial sweeteners can affect insulin sensitivity. A 2020 study in Cell Metabolism found that consuming sucralose with carbohydrates reduced insulin sensitivity in healthy participants. This underscores the importance of prioritising whole, minimally processed foods.
Monitor your progress. Regular fasting insulin tests can track how your body responds to dietary changes. For instance, reducing refined carbs may lead to noticeable improvements in just a few weeks.
While diet is essential, other lifestyle factors like exercise, sleep, and stress management are equally important for improving insulin sensitivity.
Exercise, sleep, and stress management
Diet often takes centre stage, but exercise, quality sleep, and stress management are just as critical for maintaining insulin sensitivity. These elements work together to support or hinder your metabolic health.
Exercise is a powerful tool for improving insulin function. Studies show that increasing weekly physical activity by just 500 calories reduces the risk of type 2 diabetes by about 9%. High-intensity interval training (HIIT) is particularly effective, especially for those dealing with poor sleep.
But you don’t need to go all out – simple habits like walking more, taking the stairs, or standing periodically throughout the day can make a real difference.
Stress is another factor to watch. Chronic stress raises cortisol levels, which interferes with insulin function and often leads to poor sleep. This creates a cycle where stress and poor sleep feed into each other, worsening insulin sensitivity.
Start small. Commit to a 20-minute walk after dinner, set a consistent bedtime, or practise 10 minutes of deep breathing daily. These small steps often build on each other, creating a positive cycle of improved habits.
Combining fasting insulin tests with CGM data
Pairing lifestyle changes with precise monitoring tools like fasting insulin tests and CGM provides a clearer picture of your metabolic health. Together, they offer insights that help fine-tune your approach.
Fasting insulin tests establish a baseline. When fasting plasma glucose levels exceed 4.9 mmol/L (about 88 mg/dL), the risk of insulin resistance and, consequently, diabetes doubles. This test gives you a concrete target to work toward with your lifestyle changes.
CGM fills in the gaps. While fasting tests provide a snapshot, CGM tracks glucose levels throughout the day. For example, you might learn that certain meals cause prolonged glucose spikes or that stress at work consistently raises your blood sugar in the afternoon. This real-time data helps you identify which interventions work best for your body.
Tailored diets based on post-meal glucose responses are more effective than generic plans. CGM data allows you to see exactly which foods and combinations stabilise your glucose levels.
AI technology takes this a step further. Modern CGM systems can use AI to analyse patterns and predict glucose levels. A pilot study in rural India showed that AI-driven interventions improved glycaemic control in prediabetic individuals by 18%. While this technology is still advancing, it highlights how data-driven insights can lead to more personalised strategies.
If you're wondering how to reverse insulin resistance and boost sensitivity, check out how to reverse insulin resistance insulin sensitivity for practical steps.
How Vively can help you spot and manage insulin resistance
Understanding insulin resistance early is key, and pairing fasting insulin tests with continuous monitoring gives you a clearer picture of your metabolic health. Vively provides real-time insights with continuous glucose monitoring (CGM), helping you see how your meals, movement, sleep, and stress impact your glucose levels throughout the day.
With Vively, you can:
- Track your daily glucose patterns to identify spikes and trends linked to insulin resistance.
- Get personalised guidance from an accredited dietitian to improve insulin sensitivity through diet and lifestyle changes.
- Monitor your progress over time, so you can take action before blood sugar or HbA1c levels rise.
By combining early testing with Vively’s CGM insights and expert support, you gain the tools to prevent long-term complications and take control of your metabolic health.
Take control of your metabolic health
Fasting insulin testing can reveal metabolic issues long before traditional markers like blood glucose and HbA1c show any signs. The numbers don't lie: in a study of 1,313 young adults, 30.5% had elevated insulin levels despite having normal blood glucose and HbA1c readings.
Even more surprising, among those with HbA1c under 5.7%, a range typically considered healthy, 10.5% still had fasting insulin levels above 15 mIU/L. This means that nearly 1 in 10 people labelled as "healthy" by standard tests were already showing early signs of insulin resistance.
Fasting insulin testing is far more sensitive than HbA1c or fasting glucose at detecting early resistance. HbA1c has a sensitivity of just 49%, while fasting glucose is even lower at 25%. These statistics highlight the value of integrating fasting insulin testing and continuous monitoring into your health routine.
When combined with continuous glucose monitoring (CGM), fasting insulin results can guide meaningful lifestyle changes. For example, a study of 2,217 participants using remote CGM saw improvements in hyperglycaemia, glucose variability, and even weight management.
Programs like Vively's CGM system make this process even more effective. By pairing real-time glucose tracking with personalised nutrition coaching, you can see exactly how your diet, exercise, and sleep habits impact your glucose levels. The coaching helps translate this data into practical, sustainable changes tailored to your body's unique needs.
It's also worth noting that a fasting plasma glucose level above 88 mg/dL (4.9 mmol/L) doubles your risk of insulin resistance. But you don’t need to wait for your levels to reach that point. Early lifestyle changes like the diet tweaks, exercise plans, and sleep strategies mentioned earlier – can significantly lower your risk of progressing to type 2 diabetes.
With clear early warning signs and actionable data, you have the tools to take charge of your metabolic health. A fasting insulin test, paired with CGM insights, can help you fine-tune your habits before lasting damage occurs. This proactive approach works seamlessly with lifestyle adjustments to reverse insulin resistance and keep type 2 diabetes at bay.
Your metabolic health is largely in your hands. The key is having the right information at the right time. Fasting insulin testing gives you that critical early insight, empowering you to act when it matters most.
FAQs
Why is fasting insulin a better early indicator of insulin resistance than fasting glucose or HbA1c?
Fasting insulin serves as a stronger early indicator of insulin resistance because it can reveal problems long before blood sugar levels or HbA1c begin to climb. Insulin resistance tends to develop slowly, and fasting insulin is often one of the first markers to signal that something is off.
Catching insulin resistance early allows for timely action to improve metabolic health and lower the chances of progressing to diabetes. On the other hand, fasting glucose and HbA1c usually only flag issues after blood sugar control has already been significantly disrupted.
How can changes to your diet and exercise routine improve insulin sensitivity and help manage or reverse insulin resistance?
Improving how your body responds to insulin often begins with small, manageable lifestyle changes. Regular exercise, whether it's walking, swimming, strength training, or yoga can make a big difference in how efficiently your body uses insulin. Try to aim for at least 150 minutes of moderate activity each week to see positive effects.
Your diet plays a key role too. Prioritise whole, nutrient-packed foods like vegetables, fruits, lean proteins, healthy fats, and fibre-rich options such as whole grains and legumes. Cutting back on added sugars and processed foods can also help keep your blood sugar steady and support better overall metabolic health.
By weaving these habits into your daily life, you can take meaningful steps toward managing blood sugar and reducing the risk of diabetes in the long run.
How does continuous glucose monitoring (CGM) help with understanding and managing insulin resistance?
Continuous glucose monitoring (CGM) offers real-time updates on how your blood sugar levels change during the day. By observing these trends, CGMs can reveal early indicators of insulin resistance, often before it becomes apparent through standard tests like fasting glucose or HbA1c.
With this information, you can tailor your diet, exercise routine, and daily habits to improve blood sugar control and lower the chances of developing diabetes. CGMs serve as a powerful resource for spotting issues early and taking charge of your metabolic health.
Why is fasting insulin a better early indicator of insulin resistance than fasting glucose or HbA1c?
Fasting insulin serves as a stronger early indicator of insulin resistance because it can reveal problems long before blood sugar levels or HbA1c begin to climb. Insulin resistance tends to develop slowly, and fasting insulin is often one of the first markers to signal that something is off.
Catching insulin resistance early allows for timely action to improve metabolic health and lower the chances of progressing to diabetes. On the other hand, fasting glucose and HbA1c usually only flag issues after blood sugar control has already been significantly disrupted.
How can changes to your diet and exercise routine improve insulin sensitivity and help manage or reverse insulin resistance?
Improving how your body responds to insulin often begins with small, manageable lifestyle changes. Regular exercise, whether it's walking, swimming, strength training, or yoga, can make a big difference in how efficiently your body uses insulin. Try to aim for at least 150 minutes of moderate activity each week to see positive effects.
Your diet plays a key role too. Prioritise whole, nutrient-packed foods like vegetables, fruits, lean proteins, healthy fats, and fibre-rich options such as whole grains and legumes. Cutting back on added sugars and processed foods can also help keep your blood sugar steady and support better overall metabolic health.
By weaving these habits into your daily life, you can take meaningful steps toward managing blood sugar and reducing the risk of diabetes in the long run.
How does continuous glucose monitoring (CGM) help with understanding and managing insulin resistance?
Continuous glucose monitoring (CGM) offers real-time updates on how your blood sugar levels change during the day. By observing these trends, CGMs can reveal early indicators of insulin resistance, often before it becomes apparent through standard tests like fasting glucose or HbA1c.
With this information, you can tailor your diet, exercise routine, and daily habits to improve blood sugar control and lower the chances of developing diabetes. CGMs serve as a powerful resource for spotting issues early and taking charge of your metabolic health.
Get irrefutable data about your diet and lifestyle by using your own glucose data with Vively’s CGM Program. We’re currently offering a 20% discount for our annual plan. Sign up here.
Next articles

Understanding the causes of insulin resistance
Unravel the mystery of insulin resistance, its causes and implications for your health. Explore evidence-based strategies to prevent and manage this condition and optimise your metabolic health.



 Share
Share Tweet
Tweet Share
Share















